Julia
- Spinal Cord Injury (SCI),
- T6, T7, Complete
Epidural Stimulation

| Treatment received | Implantation site | Number of devices | Duration of stay |
|---|---|---|---|
| Epidural Stimulation | Lumbar spinal cord | 1 | 35 days |
| Post-surgical care | Total sessions | Sessions per week | Time (Hr.) per session |
|---|---|---|---|
| Mapping | 90 | 20 | 1 |
| Physical therapy | 26 | 5 | 1 |
| Total sessions of rehabilitation | 116 |
| Muscle improvement | Before ES surgery | At discharge (35 days after ES surgery) |
|---|---|---|
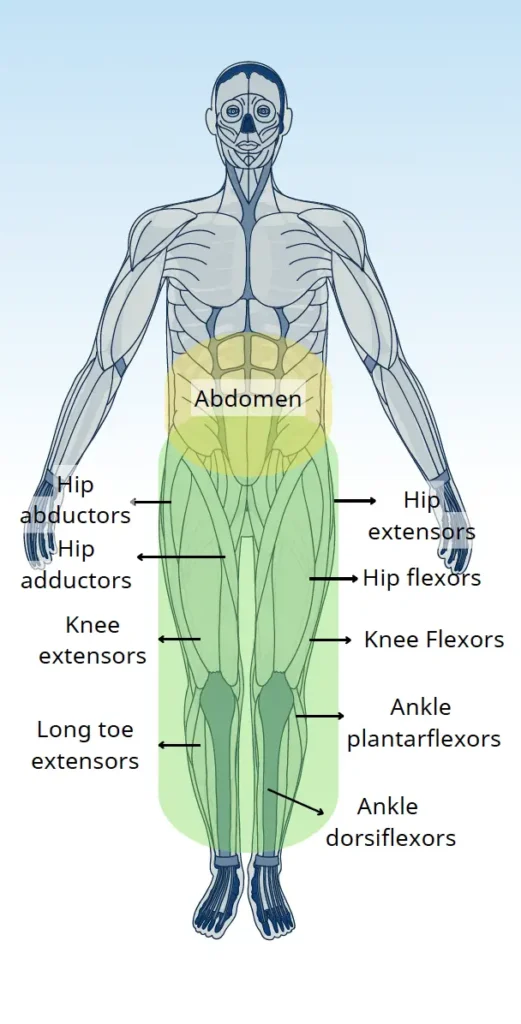
| Hip flexors | 0 | 4 |
| Hip extensors | 0 | 2 |
| Hip abductors | 0 | 2 |
| Hip adductors | 0 | 2 |
| Knee extensors | 0 | 4 |
| Knee flexors | 0 | 4 |
| Ankle dorsiflexors | 0 | 3 |
| Ankle Plantarflexors | 0 | 2 |
| Long toe extensors | 0 | 2 |
| Abilities & Symptoms | Before ES surgery | At discharge (35 days after ES Surgery) |
|---|---|---|
| Standing with support | Not possible | Possible |
| Stepping with support (for more than 10 meters) | Not possible | Possible |
| Standing balance | Absent * | Fair * |
| Sitting balance | Poor * | Good * |
| Motor coordination (while stepping) | Poor * | Good * |
| Sit to stand (in a walker) | Maximum assistance | Moderate assistance |
| Ability to transfer | Maximum assistance | Minimum assistance |
| Ability to use abdominal muscles during bowel program | Not possible | No change |
| Stamina & Fatigue | Poor * | Endurance increased |
| Spasticity | Moderate | Decreased |
| Abilities & Symptoms | Before ES surgery | At discharge (35 days after ES Surgery) |
|---|---|---|
| Neuropathic pain | Severe | Significantly decreased |
| Temperature sensations | No sensation (below the level of injury) | Slightly improved |
| Proprioception | Absent | Present |
| Bladder sensation | Absent | No change |
| Bowel sensation | Absent | No change |
| Abilities & Symptoms | Before ES surgery | At discharge (35 days after ES Surgery) |
|---|---|---|
| Sweating ability | No | Improved (on legs while stepping) |
| Temperature regulation | Poor * | Improved |
| Blood Pressure Regulation | Stable | Stable |
Julia reported significant improvements among all motor areas. After the treatment she was able to stand and walk with the help of a standing frame. She also had better sitting balance, standing balance and postural stability.
Julia reported improved proprioception and she was able to feel her lower limbs again for the first time since her injury. She also reported mild improvements in the temperature sensation below the level of injury.
Julia was able to sweat and reported better body temperature regulation after the treatment.
Significant improvements were reported in her sitting balance and trunk stability while in the sitting position.
She was able to stand in the standing frame, which was not possible before.
Julia underwent Epidural spinal cord Stimulation surgery at the lumbar spinal cord site. Her total stay was 35 days. In the first week, she had extensive check-ups, MRI scans, and surgery without complications or side effects.
Two days post surgery, Julia began the mapping program and intensive rehabilitation. She regained volitional muscle function for the first time since her injury. Gradual improvements in motor functions were seen in the second week, along with standing and walking training throughout her 35 days of treatment.
Julia’s motor function improved gradually, enabling her to stand and walk. Her balance, coordination, muscle mass, strength, and overall quality of life all showed remarkable improvement, while spasticity and neuropathic pain levels decreased.
We use cookies on our website to give you the most relevant experience by remembering your preferences and repeat visits. By clicking “Accept All”, you consent to the use of ALL the cookies. However, you may visit "Cookie Settings" to provide a controlled consent.