Dominique
- Spinal Cord Injury (SCI),
- C6, C7, Incomplete
Epidural Stimulation

| Treatment received | Implantation site | Number of devices | Duration of stay |
|---|---|---|---|
| Epidural Stimulation | Lumbar spinal cord | 1 | 35 days |
| Post-surgical care | Total sessions | Sessions per week | Time (Hr.) per session |
|---|---|---|---|
| Mapping | 90 | 20 | 1 |
| Physical therapy | 24 | 5 | 1 |
| Total sessions of rehabilitation | 114 |
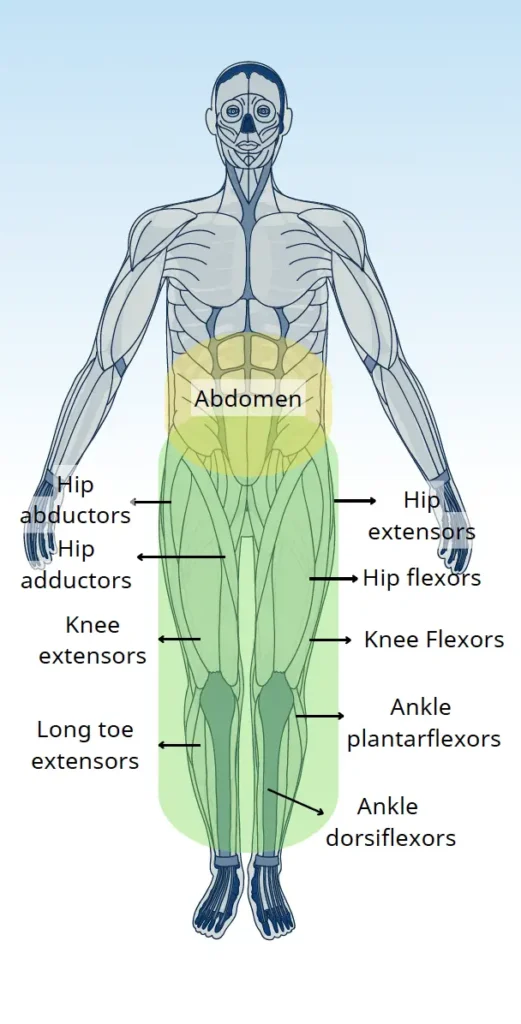
| Muscle improvement | Before ES surgery | At discharge (35 days after ES surgery) |
|---|---|---|
| Hip flexors | 2 | 4 |
| Hip extensors | 2 | 4 |
| Hip abductors | 2 | 3 |
| Hip adductors | 2 | 3 |
| Knee extensors | 2 | 3 |
| Knee flexors | 2 | 3 |
| Ankle dorsiflexors | 1 | 3 |
| Ankle plantarflexors | 2 | 3 |
| Long toe extensors | 2 | 2 |
| Abilities & Symptoms | Before ES surgery | At discharge (35 days after ES surgery) |
|---|---|---|
| Standing with support | Unable | Able (with 30% body weight) |
| Stepping with support (for more than 10 meters) | Able (with robotic gait) | Able (with Lite Gait) |
| Standing balance | Not tested | Not tested |
| Sitting balance | Good | No change |
| Motor coordination (while stepping) | Independent (with moderate assistance) | Independent (with minimal assistance) |
| Sit to stand (in a walker) | Unable | No change |
| Ability to transfer | Unable | Maximum assistance |
| Ability to use abdominal muscles during bowel program | Able (contract abdominal muscle) | Able (better abdominal muscle contraction) |
| Stamina & Fatigue | Easily tired | Better endurance |
| Spasticity | Minimal | Minimal (less than before ES surgery) |
| Abilities & Symptoms | Before ES surgery | At discharge (35 days after ES surgery) |
|---|---|---|
| Neuropathic pain | Absent | No change |
| Temperature sensations | Normal | Normal |
| Proprioception | Normal | Normal |
| Bladder sensation | Absent | No change |
| Bowel sensation | Impaired | No change |
| Abilities & Symptoms | Before ES surgery | At discharge (35 days after ES surgery) |
|---|---|---|
| Sweating ability | Absent | No change |
| Temperature regulation | Abnormal (always cold) | Normal |
| Blood pressure regulation | Abnormal (easily cold) | Normal |
With further mapping, Daemen continued to improve to an extend where she regained the ability to stand, lock both knees and able to walk in a walker. Her balance, coordination, and control over the movements improved significantly.
In terms of sensory functions, there were improved sensations in her lower limbs. Since Damen already had certain level of sensory function in her lower limbs, the recovery in sensory function was not as visible as in her muscle functions.
After the treatment she could stand for a whole 1 hour without having any issues.
Her sitting balance improved significantly after the treatment. During the mapping process, she received mapping specifically targeting her abdominal and paraspinal muscles. Her static, as well as dynamic sitting balance improved.
Due to improved trunk control, Daemen’s standing balance also improved. She would hold herself much better when walking or standing.
Dominique sustained a traumatic spinal cord injury after a fall in 2023 resulting in complete loss of muscle function in her lower limbs. She received conventional physical therapy and occupational therapy and managed to improve her upper body functions, however her lower limb functions remained a major concern.
She received the Epidural spinal cord stimulation surgery for her lower limb functions. After the surgery for ES implantation, she had a normal recovery from the surgery and 2 days later she started mapping. During the mapping process, her muscle functions started to return which continued to improve gradually over the whole course of her stay.
At the end of the treatment, Dominique showed remarkable recovery in her motor functions, the best among all the affected areas. As soon as the stimulator was turned on, there was an immediate muscle contraction. She also reported significant improvements in her sitting and standing balance and her autonomic functions. She regained the ability to stand, lock both knees and ultimately walk with support. Also, before the treatment, she suffered from postural hypotension where her blood pressure would drop just a few minutes into standing which significantly limited her ability to perform any meaningful level of body weight training. But, after receiving the treatment, she was able to stand for a whole 1 hour. This improved her ability to focus on her recovery in other areas without worrying about suffering from low blood pressure anymore.
We use cookies on our website to give you the most relevant experience by remembering your preferences and repeat visits. By clicking “Accept All”, you consent to the use of ALL the cookies. However, you may visit "Cookie Settings" to provide a controlled consent.