Benaya
- Spinal Cord Injury (SCI),
- C5, C6, C7, Incomplete
Epidural Stimulation

| Treatment received | Implantation site | Number of devices | Duration of Stay |
|---|---|---|---|
| Epidural Stimulation | Cervical spinal cord | 1 | Extened stay for neurorehabilitation (until April 2024) |
| Epidural Stimulation | Lumbar spinal cord | 1 | Extened stay for neurorehabilitation (until April 2024) |
| Post-surgical care | Date | Total sessions | Sessions per week | Time (Hr.) per session |
|---|---|---|---|---|
| Physical Therapy & Lower Extremity Mapping | 50 days after admission | 102 | 15 | 1 |
| Occupational Therapy & Upper Extremity Mapping | 50 days after admission | 69 | 10 | 1 |
| Physical Therapy & Lower Extremity Mapping | Extended stay | 614 | 20 | 1 |
| Physical Therapy & Lower Extremity MappingPhysical Therapy & Lower Extremity Mapping | Extended stay | 343 | 10 | 1 |
| Muscle improvement | Before ES surgery | At discharge (50 days after admission) | 18 months after discharge |
|---|---|---|---|
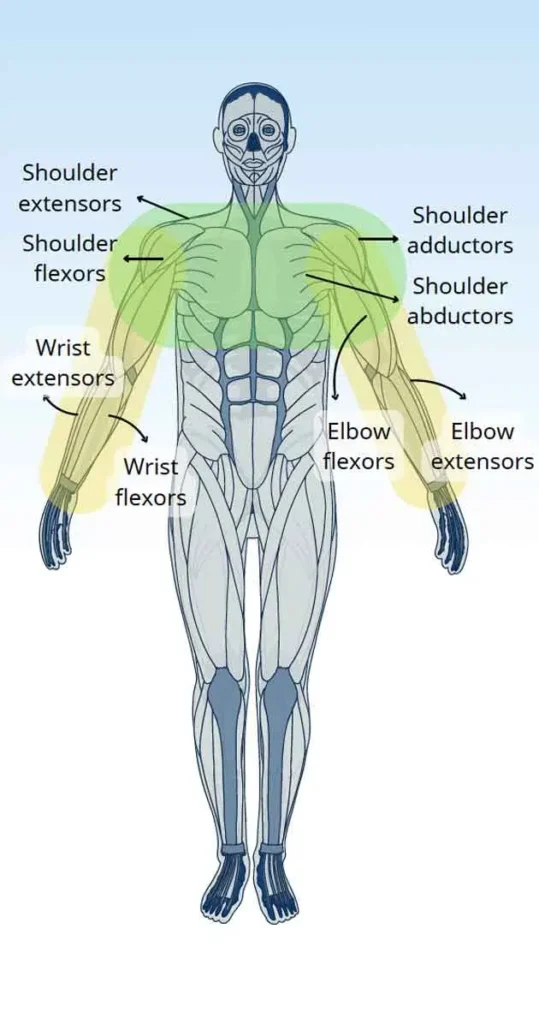
| Shoulder flexors | 1 | 1+ | 2+ |
| Shoulder extensors | 1+ | 2 | 3 |
| Shoulder abductors | 1 | 2+ | 2+ |
| Shoulder horizontal abductors | 2 | 3 | 3 |
| Shoulder adductors | 1 | 2+ | 3 |
| Shoulder horizontal adductors | 1 | 1+ | 2 |
| Shoulder flexors | 2+ | 2+ | 3+ |
| Shoulder extensors | 1 | 1+ | 1+ |
| Wrist flexors | 1 | 1 | 1+ |
| Wrist extensors | 2+ | 2+ | 2+ |
| Finger flexors | 1 | 1 | 1+ |
| Finger extensors | 0 | 1+ | 1+ |
| Muscle improvement | Before ES surgery | At discharge (50 days after admission) | 18 months after discharge |
|---|---|---|---|
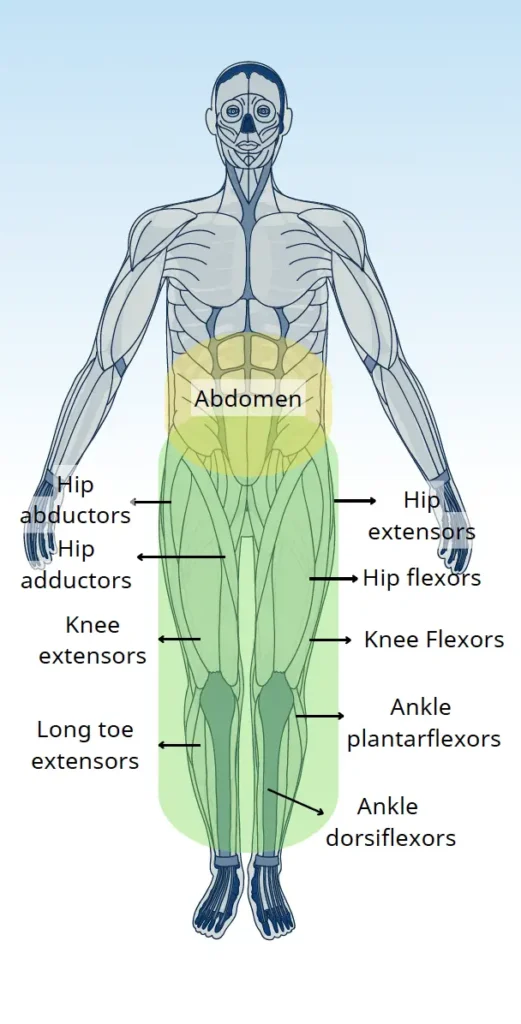
| Hip flexors | 0 | 3 | 5 |
| Hip extensors | 0 | 3 | 5 |
| Hip abductors | 0 | 2 | 2 |
| Hip adductors | 0 | 2 | 2 |
| Knee extensors | 0 | 3 | 5 |
| Knee flexors | 0 | 2 | 5 |
| Ankle dorsiflexors | 0 | 3 | 5 |
| Ankle plantarflexors | 0 | 2 | 3 |
| Long toe extensors | 0 | 2 | 2 |
| Abilities & Symptoms | Before ES surgery | At discharge (50 days after admission) | 18 months after discharge |
|---|---|---|---|
| Feeding | Not possible | Improved (able to hold large handle with strap, but bring to mouth unstably) | Improved (able to hold large handle with strap, but bring to mouth stably) |
| Grooming (personal hygienic care) | Not possible | No Change | No Change |
| Dressing | Maximal assistance (able to lift arms for caregiver) | Improved (able to lift arms higher for caregiver) | No Change |
| Writing | Not possible | No Change | No Change |
| Grasping | Not possible | Improved (able to squeeze, hold and grasp objects) | Improved (able to squeeze, hold, grasp and pinch objects) |
| Wheelchair Control (powered wheelchair) | Independent (able to control by himself) | Independent (able to control by himself) | Independent (able to control by himself) |
| Standing with support | Absent * | Poor * | Good * |
| Stepping with support (for more than 10 meters) | Absent * | Fair * | Good * |
| Standing balance | Absent * | Poor * | Fair * (moderate support) |
| Sitting balance | Poor * | Fair * | Good * |
| Motor coordination (while walking) | Absent * | Fair * | Good * |
| Sit to stand (in walker) | Absent * | Poor * | No Change |
| Ability to transfer | Absent * | Poor * | No Change |
| Ability to use abdominal muscles during bowel program | Absent * | Poor * | No Change |
| Stamina & Fatigue | Poor endurance | Fair endurance | Good endurance |
| Spasticity | Minimal spasticity | Moderate spasticity (controllable and profitable to strengthen movement) | No Change |
| Abilities & Symptoms | Before ES surgery | At discharge (50 days after admission) | 18 months after discharge |
|---|---|---|---|
| Neuropathic pain | Absent * | Absent * | Absent * |
| Temperature sensations | Absent * | No change | No change |
| Proprioception | Absent * | No change | No change |
| Bladder sensation | Absent * | No change | No change |
| Bowel sensation | Absent * | No change | No change |
| Abilities & Symptoms | Before ES surgery | At discharge (50 days after admission) | 18 months after discharge |
|---|---|---|---|
| Sweating ability | Absent * | No change | No change |
| Temperature regulation | Fair * | Normal * | Normal * |
| Blood pressure regulation | Fair * | Normal * | Normal * |
There was significant motor function gains in Benaya’s upper and lower limbs with improved muscle mass, mass tone, and overall strength.
After the treatments and long term training, Benaya started to regain proprioception. He started to feel his limbs in space and time which greatly helped him improving and control his overall walking ability.
Benaya had significant improvements to his autonomic functions including blood pressure and body temperature regulations.
He regained significant trunk stability, core muscle function and paraspinal muscles. This significantly improved his sitting balance, improved his overall posture, and reduced the risk of potential scoliosis or any structural deformity. He is able to sit and control his abdominal muscles and his dynamic sitting balance is significantly improved even when challenged.
Benaya is able to stand, lock his knees and stay upright for prolonged periods of time. His standing balance has been improving significantly.
Benaya sustained a severe and life-altering spinal cord injury, primarily from the C5 to C7 levels and his MRI scan showed severe cystic changes in his spinal cord. The injury resulted in almost complete loss of upper limb and complete loss of limb functions meaning he was fully dependent on all activities of his daily living. After a comprehensive medical evaluation, he went through the implantations of cervical and lumbar Epidural Stimulations surgeries. Both surgeries were performed together on the same day. After the surgery, he took 2 days to recover before starting the mapping process.
Immediately after the implantation of the spinal cord stimulator, his motor function started to improve as shown by the contractions in previous dormant muscle groups that consistently strengthened as we moved forward with more extensive training. His upper limbs shows improved proximal and distal muscle function. He started to train how to feed and drink by himself and reported improved finger, wrist, and arm functions. For the first time since his injury, we saw muscle contractions and motor function coming back in his lower limbs. Both flexor and extensor groups improved. Eventually, he was able to stand up, maintain postural stability in a standing position, and walk with upper body support without anyone requiring to lock his knees. His blood pressure levels became very stable and in the last 2 years, he never reported any major fluctuations. He does not suffer from postural hypotension anymore. His body temperature regulation improved. He is now able to stand and perform locomotor training for two hours or more without going through any kind of body temperature irregulation and any major fluctuations in his blood pressure levels.
Benaya has been staying with us for more than 2 years now and consistently improving. The major recovery is in his motor functions, both upper and lower limbs including the ability to stand and walk. He is also learning to perform the activities of his daily life (ADLs) by himself.
We use cookies on our website to give you the most relevant experience by remembering your preferences and repeat visits. By clicking “Accept All”, you consent to the use of ALL the cookies. However, you may visit "Cookie Settings" to provide a controlled consent.