Spinal cord injury and UTIs often go hand in hand. Neurogenic bladder dysfunction is among the leading problems in patients suffering from both complete and incomplete spinal cord injury. It results in impairments in storage and voiding capacity and results in frequent urinary tract infections (UTIs) in this group of patients. Patients with clinically complete spinal cord injuries often require intermittent or indwelling catheters, further increasing the chances of UTIs. In SCI patients, UTIs are a leading cause of septicemia and result in a higher risk of mortality. Moreover, UTIs significantly impair the quality of life and have serious socio-economic consequences.
What are UTIs?
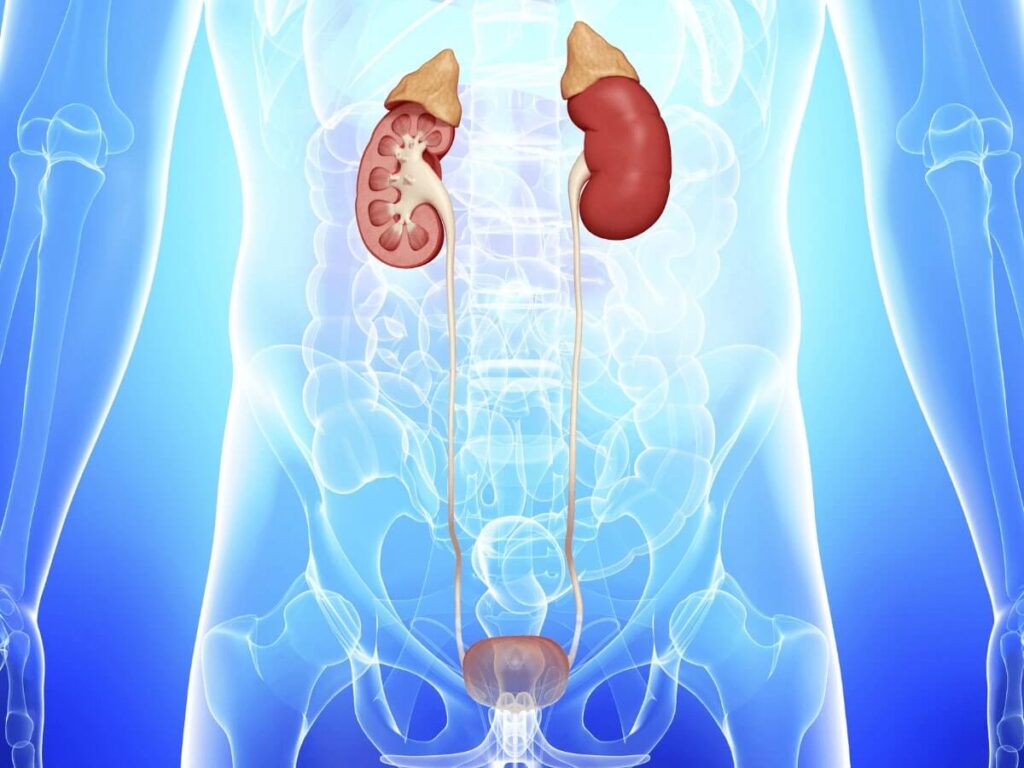
A urinary tract infection, or UTI, is an umbrella term for infections which affect any part of the urinary tract, including the kidneys, ureters, bladder and urethra. The majority of UTIs impact the lower part of this system, the bladder and the urethra. In patients with sensory function in the lower body, infections can cause discomfort but more common impacts for spinal cord injury patients include:
- Impaired or reduced bladder capacity
- Urinary Incontinence
- Impaired bladder emptying
- Permanent or intermittent catheterization
- Poor personal hygiene
- Compromised immune system
What Are The Risks Around Spinal Cord Injury and UTIs?
UTIs are more common in spinal cord injury patients, largely due to the loss of normal bowel and bladder function. The risk of bacteria entering the urethra increases when bladder and bowel management occurs. From there, the bacteria move into the bladder, causing bladder infections. Once in the bladder, this bacteria is hard to get rid of. People with spinal cord injury can’t fully empty their bladder, which means that bacteria stays and thrives in the bladder, causing UTIs. The risk of UTIs in spinal cord injury patients are:
Bacteremia, Septicemia and increased risk of systemic complications
If bacteria from a UTI enters the bloodstream it can cause a host of problems. Bacteremia, when bacteria enter the blood, can cause Septicemia if untreated, where the bacteria multiply. Septicemia is potentially fatal.Cystitis and Kidney infections
UTIs can also escalate into more serious infections of the urinary tract, such as cystitis (bladder inflammation) or kidney infections. If untreated, kidney infections can lead to dangerous complications such as kidney failure or septicemia, which can be fatal.Multiple Organ Failures
Septicemia becomes fatal when it causes the organs to begin shutting down after the blood flow to them is impaired.Acute Kidney Failure
Acute kidney failure requires urgent treatment in order to prevent it from becoming fatal. Even if treated it can cause permanent damage to the kidneys, especially in patients who have pre-existing conditions.Permanent Kidney damage
Following kidney failure, patients can be left with permanent kidney damage. This creates a risk of the kidneys not functioning properly and leaving waste products and fluid in the body.
Treatments And Prevention
The European and US FDA guidelines for treating UTIs include the use of appropriate antibiotics, either by oral or IV route. Patients who are at significantly increased risk of UTIs, such as SCI patients, are also prescribed prophylactic antibiotics. Patients and their caregivers are educated on using proper sterile techniques while performing intermittent or indwelling catheterizations and improved personal hygiene. Patients with hyperactive bladder syndrome are being prescribed a separate group of drugs in order to reduce the risk of urinary incontinence.
Epidural spinal cord stimulation in SCI patients has been associated with improving the neurogenic bowel function by increasing and regulating the bladder’s contractile mobility. This improves the voiding capacity of the bladder, which can reduce the risk of UTIs in these patients.
Epidural spinal cord stimulation in SCI patients has been associated with improving the neurogenic bowel function by increasing and regulating the bladder’s contractile mobility. This improves the voiding capacity of the bladder, which can reduce the risk of UTIs in these patients.
References
- Goetz LL, Klausner AP. Strategies for Prevention of Urinary Tract Infections in Neurogenic Bladder Dysfunction. Phys Med Rehabil Clin N Am. 2014;25:605–618.
- Cardenas DD, Hooton TM. Urinary tract infection in persons with spinal cord injury. Arch Phys Med Rehabil. 1995;76:272–280.
- Esclarin DRA, Garcia LE, Herruzo CR. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol. 2000;164:1285–1289.
- Grabe M, Bishop MC, Bjerklund-Johansen TE, et al. Peri-operative antibacterial prophylaxis in urology: guidelines on the management of urinary and male genital tract infections. Arnhem, The Netherlands European Association of Urology; 2008: 90- 100.
- Gürbüz B, Güner B, Atis G, et al. Are prophylactic antibiotics necessary for urodynamic study? Kaohsiung J Med Sci. 2013;29:325–329.
- Bennett JK, Gray M, Green BG, Foote JE. Continent diversion and bladder augmentation in spinal cord injured patients. Semin Urol. 1992;10:121–132.
- Waites KB, Canupp KC, Brookings ES, DeVivo MJ. Effect of oral ciprofloxacin on bacterial flora of perineum, urethra, and lower urinary tract in men with spinal cord injury. J Spinal Cord Med 1999;22(3):192–8






