After any kind of spinal cord pathology, the majority of patients suffer from neurogenic bladder dysfunction. Whether the injury is traumatic or non-traumatic, both the bowel and bladder are normally affected. Loss of control of bladder function results in urinary incontinence, urinary retention, renal impairment and increased likelihood of kidney stones. It is hard to treat neurogenic bladder dysfunction, but we have seen some success with our epidural stimulation treatment.
How SCI Affects Bladder Function
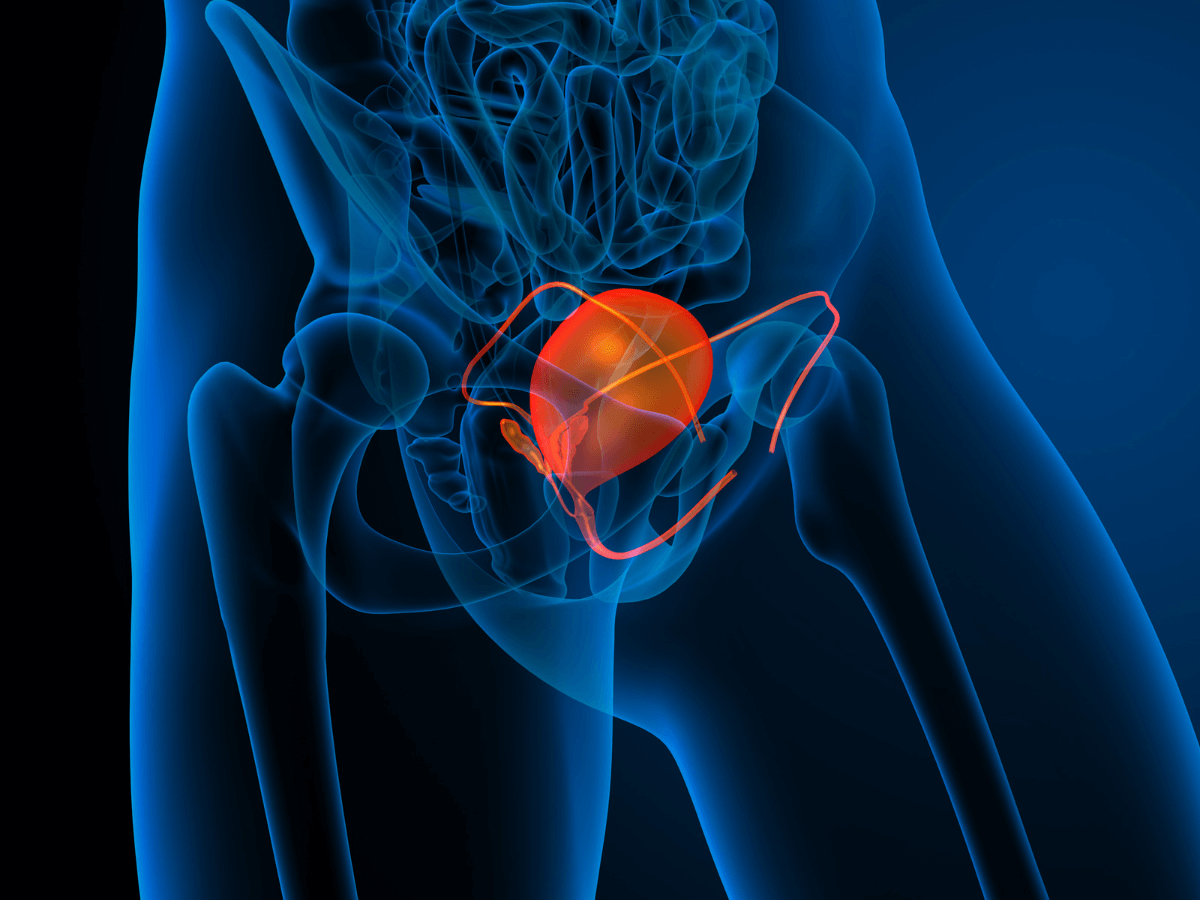
To understand how SCI affects the bladder function, it is important to first understand how a typical bladder functions. Urinary function requires a coordinated effort between our micturition center (located in the brainstem), our autonomic nervous system (ANS) and our bladder muscles and sphincters. Both the sympathetic and parasympathetic components of the ANS are involved in bladder regulation. The sympathetic component is responsible for our fight and flight response, preparing the body for physical activity. The parasympathetic stimulates the ‘rest and digest’ and the ‘feed and breed’ responses, or the basic bodily functions.
Sympathetic Activity
The sympathetic stimulation of the bladder originates from the lower thoracic and upper lumbar spinal cord segments, between the T10-L2 levels.
As urine accumulates in the bladder, it leads to a modest increase in bladder pressure. This activates the sympathetic stimulation, which closes the internal sphincter and inhibits the contraction of the bladder wall muscles, allowing the bladder to fill. At the same time, the stretching of the bladder as it fills inhibits parasympathetic activity, which would otherwise contract the bladder and allow the internal sphincter to open.
When the bladder is full, sensory nerve activity conveys this information to the micturition center in the brainstem. Parasympathetic tone is increased and sympathetic activity is decreased, causing the internal sphincter muscle to relax and the bladder to contract and empty.
As urine accumulates in the bladder, it leads to a modest increase in bladder pressure. This activates the sympathetic stimulation, which closes the internal sphincter and inhibits the contraction of the bladder wall muscles, allowing the bladder to fill. At the same time, the stretching of the bladder as it fills inhibits parasympathetic activity, which would otherwise contract the bladder and allow the internal sphincter to open.
When the bladder is full, sensory nerve activity conveys this information to the micturition center in the brainstem. Parasympathetic tone is increased and sympathetic activity is decreased, causing the internal sphincter muscle to relax and the bladder to contract and empty.
Parasympathetic Activity
The parasympathetic control of the bladder muscle originates with neurons in the sacral spinal cord segments, between levels S2–S4. These neurons control the motor neurons located in or close to the bladder wall.
Sensory receptors in the bladder wall supply information to the spinal cord and to higher autonomic centers in the brainstem. These centers in turn project information to the various central coordinating centers for bladder function in the brainstem. Thus the sympathetic nervous system prevents the premature contraction and opening of the bladder, allowing it to get full. Once the bladder is filled, the parasympathetic system takes over and allows it to contract and open.
Sensory receptors in the bladder wall supply information to the spinal cord and to higher autonomic centers in the brainstem. These centers in turn project information to the various central coordinating centers for bladder function in the brainstem. Thus the sympathetic nervous system prevents the premature contraction and opening of the bladder, allowing it to get full. Once the bladder is filled, the parasympathetic system takes over and allows it to contract and open.

Somatic Nervous System Activity
The neurons which support voluntary control of the ureteral sphincter are also located in the sacral spinal cord segments, between the S2–S4 levels.
As the bladder fills these neurons are active, keeping the external sphincter closed and preventing bladder from emptying. They remain active until circumstances permit urination. In other words, it is these neurons which mean you can wait until you get to the toilet before you urinate.
During urination, or “voiding,” as clinicians often call this process, the neural activity is temporarily inhibited, leading to relaxation in the external sphincter muscle. This coordinated effort between autonomic and voluntary motor systems allows for a smooth and controllable urinary function.
After a traumatic or non-traumatic spinal injury, the autonomic and voluntary motor function fibers are disrupted. This makes them unable to provide enough stimulation to those lower parts of the spinal cord which regulate bladder function. Moreover, the normal sensory feedback loop is severely impaired which prevents the micturition center in the brainstem from providing normal coordination between the sympathetic and parasympathetic nervous systems. As a result the bladder functions become partly or entirely out of control depending upon the nature and location of the injury.
As the bladder fills these neurons are active, keeping the external sphincter closed and preventing bladder from emptying. They remain active until circumstances permit urination. In other words, it is these neurons which mean you can wait until you get to the toilet before you urinate.
During urination, or “voiding,” as clinicians often call this process, the neural activity is temporarily inhibited, leading to relaxation in the external sphincter muscle. This coordinated effort between autonomic and voluntary motor systems allows for a smooth and controllable urinary function.
After a traumatic or non-traumatic spinal injury, the autonomic and voluntary motor function fibers are disrupted. This makes them unable to provide enough stimulation to those lower parts of the spinal cord which regulate bladder function. Moreover, the normal sensory feedback loop is severely impaired which prevents the micturition center in the brainstem from providing normal coordination between the sympathetic and parasympathetic nervous systems. As a result the bladder functions become partly or entirely out of control depending upon the nature and location of the injury.
How Epidural Spinal Cord Stimulation Helps
Epidural stimulation reactivates the autonomic and motor neurons located at the lower thoracic and sacral spinal cord levels. This activation enhances their function. We have noticed that long term spinal cord stimulation modulates the function of spinal cord segments directly responsible for the autonomic and motor nerve supply. By extension, control over the bladder is improved, as well as the internal and external urinary sphincters. This allows the patient to regain a certain level of voiding function, reduces the incidences of urinary incontinence and reduces the incidence rate of secondary complications such as urinary tract infections and bladder stones.
References
- Jamil, F. Towards a catheter free status in neurogenic bladder dysfunction: a review of bladder management options in spinal cord injury (SCI). Spinal cord. 39:355–361 (2001).
- Behrman, A. L. et al. Locomotor training progression and outcomes after incomplete spinal cord injury. Physical therapy. 85:1356–1371 (2005).
- Herrity, A.N. et al. Lumbosacral spinal cord epidural stimulation improves voiding function after human spinal cord injury, Scientific Reports. 8:8688 (2018).
- Hull R. et. al. Urinary tract infection prophylaxis using Escherichia coli 83972 in spinal cord injured patients. J Urol. 163(3):872-7 (2000).
- Buczyński AZ. Principles for urological management of SCI patients. Ortop Traumatol Rehabil. 2(1):57-60 (2000).
- Pardee C, Bricker D, Rundquist J, MacRae C, Tebben C. Characteristics of neurogenic bowel in spinal cord injury and perceived quality of life. Rehabil Nurs. 37(3):128-35 (2012).