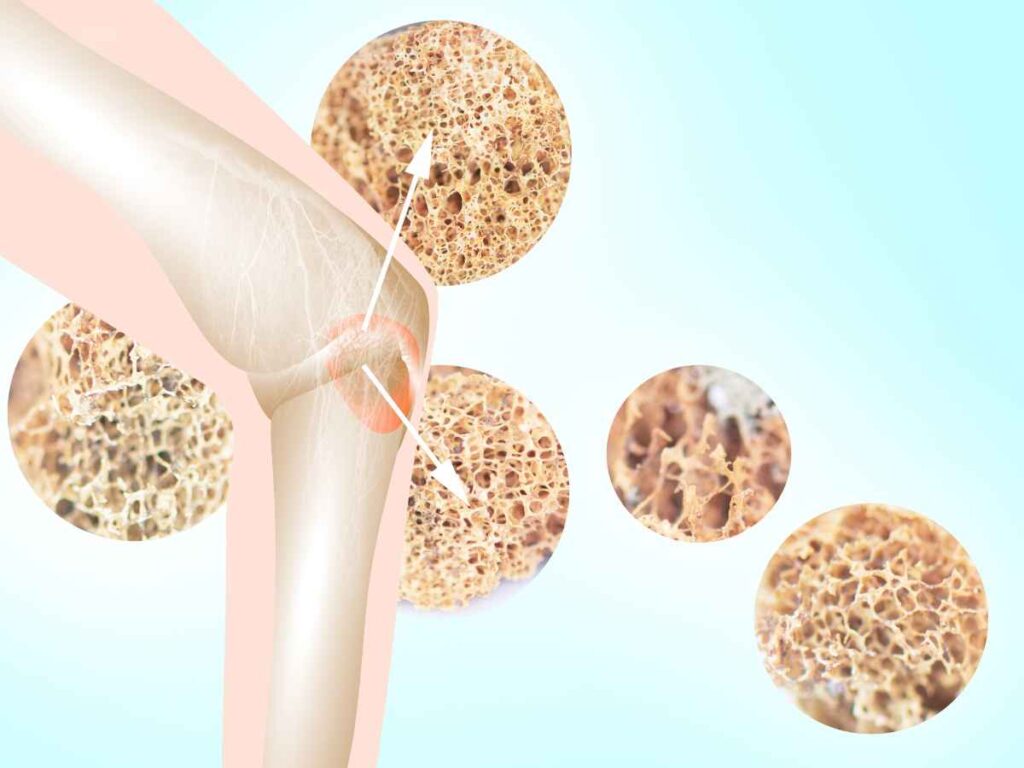
Osteoporosis after spinal cord injury (SCI) is extremely common. More than 50% of the patients with a complete spinal cord injury develop osteoporosis within 1st year of the injury and the prevalence rates go as high as 80% in long-term SCI patients. Osteoporosis is a medical condition describing overall compromised bone strength as a result of reduced bone mineral density (BMD). Osteopenia, a moderate loss in BMD, and osteoporosis, a severe loss in BMD, are among the most common long-term complications after a severe traumatic or non-traumatic spinal cord injury. Osteoporosis often is a major limiting factor in rehabilitation settings and results in frequent fractures in many patients during transfers or during bodyweight training. However, at Verita Neuro, many patients see improvements in this area as a result of both epidural stimulation treatment and stem cell treatment.
Why Do Patients Develop Osteoporosis After Spinal Cord Injury?
Osteopenia and Osteoporosis from disuse
Spinal cord injury patients with complete or severe spinal cord injuries often undergo prolonged periods of immobilization resulting in the disuse and weakness of bone strength. Normal maintenance of bone strength requires an active remodeling of bone formation and bone resorption. When SCI patients undergo prolonged periods of immobilization and no weight bearing this results in decoupling of this remodeling process, resulting in loss of bone mass and bone density.
Sclerostin, Vitamin D, Parathyroid Hormone
Sclerostin is a protein, produced by a type of bone cell, which inhibits bone growth. It plays an important role in SCI-induced bone loss. Recent studies indicated that prolonged periods of immobilization and lack of body weight training results in increased levels of sclerostin which in turn results in loss of BMD. Moreover, sclerostin levels appear to be highest during the initial post-injury phase, followed by decreasing levels detected in chronic SCI osteoporosis patients.
Also, SCI patients have moderately or sometimes severely low levels of vitamin D and parathyroid hormones, both of which are extremely important in active remodeling and bone health. Vitamin D is vital in absorption of calcium and parathyroid hormone stimulates bone remodeling by increasing the activity of bone resorption.
Long-Term Implications
Studies have shown that a few weeks after the SCI, the regions below the level of injury experience an estimated 4% BMD loss per year. Furthermore, the long bones, particularly in lower limbs continue to get thinner at a greater rate, putting patients at higher risk of femur or tibial fractures.
Treating and Managing Osteoporosis.
Body Weight Training
Weight-bearing activity stimulates and creates an ideal stress environment to promote physiologic bone remodeling. Mechanical loading has demonstrated reversal capabilities in the SCI-induced osteoporotic process in long bones in the lower extremities. Specifically, cortical thickening is noted in response to applied mechanical stress and strain even after disuse osteopenia has occurred. Cortical bone tissue is that which forms a protective layer around the internal cavity and makes up 80% of the total mass of the human skeleton.
Calcium and Vitamin D
All SCI patients should take calcium and vitamin D supplementation. Patients should be educated on the recommended daily intake, as supplementation plays a critical role in maintaining bone health.

Pharmacology Therapy
In patients at severe risk of falls and stress fractures, pharmacological therapies are essential. There are multiple therapeutic options available, depending on the cause of the osteopenia and other factors related to the patient’s general health and hormonal considerations.
Epidural Spinal Cord Stimulation and Bone Health
Epidural stimulation is used to restore muscle function and voluntary motor activity in patients with severe spinal cord injury. Patients who receive epidural stimulation treatment usually regain the use of upper and lower extremities, which greatly enhances their ability to perform body-weight training. Many patients undergo 10-15 hours of body weight training per week after the implantation of the epidural stimulation. This greatly enhances the recovery of bone health and BMD.
Stem Cell Treatment and Bone Health
As part of the Verita Neuro treatment protocol, a great majority of our patients receive mesenchymal stem cell therapy along with spinal cord stimulation. Mesenchymal stem cells have shown to play an important role in bone remodeling, due to their paracrine and secretary effects.
References
- Szollar, S. M., Martin, E. M., Sartoris, D. J., Parthemore, J. G., & Deftos, L. J. (1998). Bone mineral density and indexes of bone metabolism in spinal cord injury. American journal of physical medicine & rehabilitation, 77(1), 28–35.
- Varacallo, M., Davis, D. D., & Pizzutillo, P. (2023). Osteoporosis in Spinal Cord Injuries. In StatPearls. StatPearls Publishing.
- Varacallo M, Seaman TJ, Jandu JS, et al. Osteopenia. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing
- Battaglino, R. A., Lazzari, A. A., Garshick, E., & Morse, L. R. (2012). Spinal cord injury-induced osteoporosis: pathogenesis and emerging therapies. Current osteoporosis reports, 10(4), 278–285.
- Frontera, J. E., & Mollett, P. (2017). Aging with Spinal Cord Injury: An Update. Physical medicine and rehabilitation clinics of North America, 28(4), 821–828.
- Gifre, L., Vidal, J., Carrasco, J. L., Muxi, A., Portell, E., Monegal, A., Guañabens, N., & Peris, P. (2015). Risk factors for the development of osteoporosis after spinal cord injury. A 12-month follow-up study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 26(9), 2273–2280.
- Varacallo, M. A., Fox, E. J., Paul, E. M., Hassenbein, S. E., & Warlow, P. M. (2013). Patients’ response toward an automated orthopedic osteoporosis intervention program. Geriatric orthopaedic surgery & rehabilitation, 4(3), 89–98.







