Poor thermoregulation after SCI is one of many acute and chronic complications which spinal cord injury survivors face. As well as the loss of motor and sensory functions, patients also lose autonomic function. Autonomic dysregulation is the cause of a patient’s inability to regulate body temperature, as the sympathetic nervous system which controls this function is affected. Like many other features of spinal cord injury, the location and severity of the injury has a direct correlation with body temperature regulation. Patients with higher level and more severe injuries tend to be more affected by their inability to regulate body temperature. This is primarily because:
- Patients with lower levels of injury tend to have more available sympathetic nerve supply, which helps with sweating and heat redistribution.
- Patients with lower levels of injury tend to have more muscle mass available for heat dissipation and consumption of oxygen.
Other factors such as respiratory and cardiovascular functions, as well as the distribution of blood supply to the skin, also play important roles. Tetraplegic patients are significantly more affected as compared to those suffering from paraplegia. This is due to a larger proportion of the body having reduced functions.
What Does Unimpeded Thermoregulation Look Like?
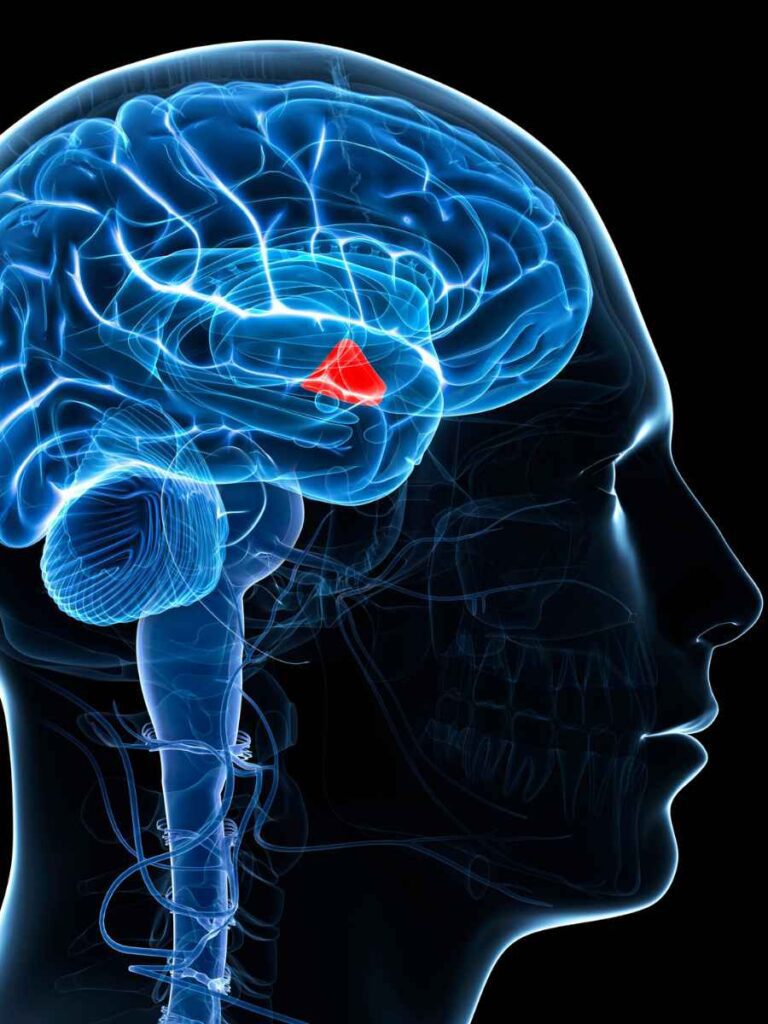
Body temperature regulation and heat dissipation & redistribution are some of the most intrinsic and important activities carried out by the nervous system. During exercise, day-to-day activities, and even at rest, the body produces a significant amount of heat as a result of metabolic activity, which needs to be regulated and redistributed. Body temperature regulation is directly controlled by the autonomic nervous system, mostly through sympathetic activity. An increase in body temperature triggers the “thermoregulator”, which is a network of neurons located in the hypothalamus in the brain. The sensory input (increased body temperature) triggers increased activity of the sympathetic nervous system. This in turn stimulates the vital organs responsible for heat dissipation, including sweat glands and blood vasculature, with blood vessels dilating. The cardiovascular and respiratory functions are also triggered.
What Happens To Thermoregulation After SCI?
Spinal cord injury affects multiple components which are required for normal body temperature regulation. First of all, due to disruption of the sensory pathways, the hypothalamus is unable to receive the appropriate sensory input which tells it the body is overly heated. Even in the presence of proper sensory input, for example in the case of an incomplete spinal cord injury, the sympathetic nervous system is partially disrupted and hence there is inefficient stimulation of vital organs responsible for heat dissipation namely sweat glands, blood vessels, and cardio-pulmonary systems. This results in impaired regulation of body temperatures in spinal cord injury patients.
How Epidural Stimulation Can Help With Thermoregulation After SCI
Epidural spinal cord stimulation for SCI is designed to provide precise electrical stimulation to various segments of the spinal cord, including the lower thoracic and lumbar spinal cord. The thoracic spinal cord contains the motor neurons responsible for sympathetic activity, including body temperature regulation. Following traumatic spinal injury, the supra-spinal input to these autonomic motor neurons is limited. By stimulating these pathways with electrical pulses, epidural stimulation results in increased excitability of the motor neurons, which allows them to perform enhanced functions.
The vast majority of our patients, after mid to long-term use of spinal cord stimulation, have reported improved body temperature regulation, even after very strenuous physical activity.
References
- Adams, T. (1971). Carnivores. In G. C. Whittow (Ed.), Comparative physiology of thermoregulation, Volume II: Mammals (pp. 151–189). New York, NY: Academic Press.
- Bain, A. R., Nybo, L., & Ainslie, P. N. (2015). Cerebral vascular control and metabolism in heat stress. Comprehensive Physiology, 5(3), 1345–1380.
- Bell, A. W., Hilditch, T. E., Horton, P. W., & Thompson, G. E. (1976). The distribution of blood flow between individual muscles and non-muscular tissues in the hind limb of the young ox (Bos taurus): Values at thermoneutrality and during exposure to cold. Journal of Physiology, 257(1), 229–243.
- Blackburn, S., Sammons, D. L., & Wilson, T. E. (2012). Palmar-plantar and axillary hyperhidrosis: Physiology, pathophysiology and treatment options. Journal of the American Osteopathic College of Dermatology, 22, 64–68.
- Brothers, R. M., Bhella, P. S., Shibata, S., Wingo, J. E., Levine, B. D., & Crandall, C. G. (2009). Cardiac systolic and diastolic function during whole body heat stress. American Journal of Physiology−Heart and Circulatory Physiology, 296(4), H1150–H1156.
- Charkoudian, N., & Wallin, B. G. (2014). Sympathetic neural activity to the cardiovascular system: Integrator of systemic physiology and interindividual characteristics. Comprehensive Physiology, 4(2), 825–850.






